Prostatitis is a disease characterized by the presence of inflammation and/or infection located in the prostate.
It can present with a wide variety of clinical signs and complaints.
Anatomy
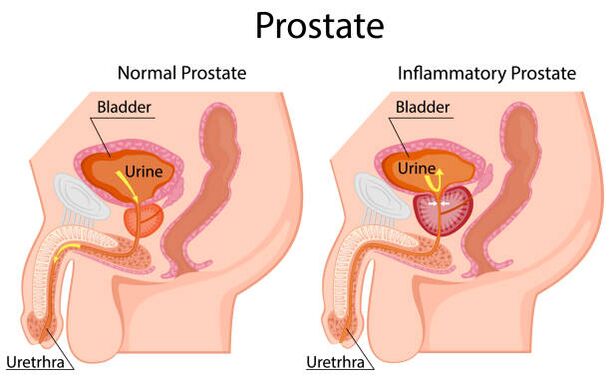
The prostate is a small gland that is part of the male reproductive system and is a hormone-dependent organ. Its shape and size have been compared to a large walnut. A normal prostate weighs about 20 g, has a volume of 15-25 ml and measures 3 cm long, 4 cm wide and 2 cm deep.
The prostate is located in the small pelvis, under the bladder and above the rectum. The urethra, the urethra, passes through the thickness of the gland. The prostate is surrounded by a capsule composed of smooth muscle, collagen and elastic fibers; covered with three layers of dense connective tissue (fascia) on the anterior, lateral, and posterior surfaces. The posterior surface of the prostate is limited by the ampulla of the rectum. They are separated by the retrovesical fascia or Denonville fascia, which allows palpation of the posterior surface of the prostate.
The prostate is composed of approximately 70% glandular tissue and 30% fibromuscular stroma. It is common to divide the organ into 3 zones.
Transition zone.The transition zone accounts for 10% of glandular tissue and 20% of cases of malignant prostate tumors. In this area, one of the main age-related diseases in men forms - benign prostatic hyperplasia, which can cause difficulty in urinating due to excessive tissue growth.
Central zone.The area around the ejaculatory ducts. It consists of glandular tissue, connective tissue and muscle elements. Tumors in this area are extremely rare.
Peripheral zone.It covers the posterior and lateral sides of the prostate and contains 70% of the glandular tissue. This is a palpable area through the rectum and allows the urologist to assess the condition of the prostate. Up to 70% of malignant tumors are located precisely in the peripheral zone. Therefore, digital rectal examination is an important diagnostic method and should be performed in patients over 45 years of age.
Prostate Functions:
- production of secretion from the prostate, which is an integral part of the sperm and is involved in the liquefaction of the ejaculate, as well as saturation with nutrients such as various enzymes and vitamins, citric acid, zinc ions, which help to improve the mobility and activity of the sperm. sperm;
- The prostate contains smooth muscle fibers that help release sperm from the urethra during ejaculation, prevent sperm from entering the bladder, and are involved in the urinary retention mechanism.
Prostatitis, benign prostatic hyperplasia and prostate cancer are the three main prostate diseases.
All three diseases can coexist in the same prostate at the same time. That is, the presence of prostatitis does not exclude the presence of prostatic hyperplasia and prostate cancer in the patient and vice versa.
Causes of Prostatitis
According to statistics, prostatitis is the most common urological disease - after hyperplasia and prostate cancer - in men under 50 and the third most common in men over 50.
Prostatitis accounts for 6 to 8% of urological outpatient visits.
The most common causative agent of prostatitis is E. coli strains, which are detected in 80% of cases. Rarer pathogens are enterococci, Pseudomonas aeruginosa, Klebsiella and other gram-negative bacteria. The role of sexually transmitted infections (such as Chlamydia trachomatis) in prostate inflammation is not yet clearly established and is under study. In patients with HIV infection and other severe changes in the immune system, possible causative agents are cytomegalovirus, Mycobacterium tuberculosis, fungi and other rare pathogens. There are data that indicate the presence of microorganisms in the prostate that are not detected in standard studies, but play a role in the appearance of inflammatory changes and the subsequent development of symptoms of prostatitis.
Possible causes of prostatitis are:
- intraprostatic reflux of urine as a result of dysfunctional urination (urine, with certain predisposing factors, can enter the prostate through the prostate ducts, causing an inflammatory process);
- unprotected anal sex;
- narrowing of the foreskin (phimosis);
- autoimmune diseases;
- functional and anatomical changes in pelvic floor muscles;
- changes in the central nervous system, including functional and anatomical changes in the brain;
- traumatic and unusual sexual activity;
- Psychological factors (in several studies, the influence of psychological stress on the occurrence of symptoms of chronic prostatitis was proven - in some patients psychosomatic disorders were diagnosed, in whose treatment a decrease in prostatitis symptoms was observed and the probability of its relapse was noted) .
Risk factors for prostatitis also include: abstinence or excessive sexual activity, refraining from ejaculation, smoking, working at night, sedentary lifestyle, inadequate fluid intake, and poor diet.
Symptoms
- pain or burning when urinating (dysuria);
- urinary disorders;
- urine discoloration;
- the appearance of blood in the urine;
- pain in the abdomen, groin or lower back;
- perineal pain;
- pain or discomfort in the penis and testicles;
- pain with ejaculation;
- increased body temperature (with acute bacterial prostatitis).
Diagnosis
According to the generally recognized NIH (US National Institutes of Health) classification of prostatitis, there are four categories of diseases, traditionally denoted by Roman numerals:
- I - acute bacterial prostatitis;
- II - chronic bacterial prostatitis;
- III - chronic bacterial prostatitis / chronic pelvic pain syndrome (CP / CPPS);
- IIIa - chronic prostatitis syndrome / chronic pelvic pain with signs of inflammation;
- IIIb - chronic prostatitis syndrome / chronic pelvic pain without signs of inflammation;
- IV - asymptomatic (asymptomatic) chronic prostatitis.
Despite the widespread prevalence of prostatitis, acute bacterial prostatitis is uncommon - 5% of all cases of the disease. But its diagnosis is quite simple, since the picture of the disease is most often pronounced: a man complains of frequent and painful urination, pain in the uterus and perineum. An increase in body temperature is characteristic, and often at high values - less than 39 °C.
The diagnosis of acute bacterial prostatitis involves a digital rectal exam (rectal exam), which involves feeling (palpating) the prostate with your index finger through the anus (rectum).
Digital rectal examination (DRE) is an important diagnostic manipulation if any prostate pathology is suspected. Therefore, it is advisable that men do not refuse to lead it.
In acute bacterial prostatitis, the prostate on palpation is acutely painful, swollen, most often enlarged. Ultrasound examination may show not only an increase in the size of the prostate, but also foci of purulent fusion of prostate tissue (abscesses) - but this happens infrequently and is usually the result of an ongoing process.
Laboratory diagnosis first includes a general urine test, in which an increase in the number of white blood cells is observed. Bacteriological urine culture is recommended. Based on the results of the analysis, it is possible to determine the presence of the bacteria and its sensitivity to the antibiotic, and thus adjust the prescribed antibiotic therapy. A general blood test is also performed to assess the general condition of the body and its response to the inflammatory process.
Taking secretions from the prostate for the diagnosis of acute prostatitis is contraindicated due to the increased risk of a life-threatening condition: bacteremia and sepsis. The determination of the oncomarker (PSA), its fractions is also not recommended - due to the low information content and data distortion in the context of inflammation.
Prostatitis treatment
Antibiotic therapy is the basic therapy for patients with prostatitis of all categories.
Alpha-blockers are also an effective group of drugs. As a result of its action, the tone of the smooth muscles of the prostate, bladder neck and prostatic part of the urethra decreases, thus improving urination and reducing the possibility of urine entering the prostate (intraprostatic urine reflux), which is one of the causes of prostatitis. The most effective and popular drugs are tamsulosin and silodosin. They are also widely used to improve urination in patients with an enlarged prostate.
It is possible to use anti-inflammatory drugs (Diclofenac), which effectively reduce pain and discomfort when urinating, reducing prostate swelling, and also contribute to some improvement in urinary quality.
Acute bacterial prostatitis is often a reason for hospitalization in a hospital, where antibiotic therapy is prescribed in the form of intravenous injections. After the patient's condition has stabilized, the patient continues to receive antibiotics in tablet form for 15 or more days in order to prevent the transition from acute to chronic bacterial prostatitis.
According to statistics, 10% of patients with acute prostatitis develop chronic bacterial prostatitis. Another 10% of patients will develop chronic pelvic pain syndrome (chronic IIIb prostatitis) in the future.
How is the treatment of prostatitis in the clinic
Urologists treat prostatitis and other diseases of the genitourinary system, based on international clinical guidelines. This means that they not only use their professional knowledge, but are also guided by scientifically proven diagnostic and therapy methods accepted around the world.
Our doctors do not prescribe ineffective medications and tests "just in case", they do not treat non-existent diseases. When making a diagnosis, the urologist trusts the data obtained from the patient's examination, the clinical picture, the data from laboratory and instrumental tests. If surgical treatment is required, a surgical operation is performed in the clinic's territory.

























